Abstract
Introduction: Despite therapeutic advances and the increasing number of available regimens, multiple myeloma (MM) remains largely incurable, with a decreased durability of response with successive therapies (Majithia et al, Leukemia 2016). The monoclonal antibodies (mAbs) daratumumab (dara) and elotuzumab (elo), targeting CD38 and SLAMF7, respectively, have demonstrated significant efficacy in relapsed/refractory (RR) MM and may lead to a paradigm change in the treatment of RRMM. In the USA, dara is indicated for the treatment of RRMM when given in combination with dexamethasone (dex) plus either lenalidomide (len; Ld) or bortezomib for patients (pts) with ≥1 prior line of therapy (LoT). Dara in combination with pomalidomide/dex (pom; Pd) was also recently approved for pts with RRMM after ≥2 prior LoTs, including len and a proteasome inhibitor (PI), on the basis of data from a single-arm trial that demonstrated a median progression-free survival of 9.9 mo (Facon et al, Blood 2017), and as a monotherapy in pts with ≥3 prior LoTs. Elo, combined with Ld, is approved for treatment of RRMM after 1-3 LoTs. In ELOQUENT-3 (NCT02654132), an ongoing phase 2 randomized study in pts with RRMM after failure of len and a PI, elo plus Pd was associated with a 46% reduction in risk of progression or death vs Pd alone (Dimopoulos et al. EHA 2018 [LB2606]). There is a lack of current data on the array of treatments received by pts with RRMM after failing mAb therapy. This study evaluated treatment sequences among pts with RRMM after failure of dara-based therapy.
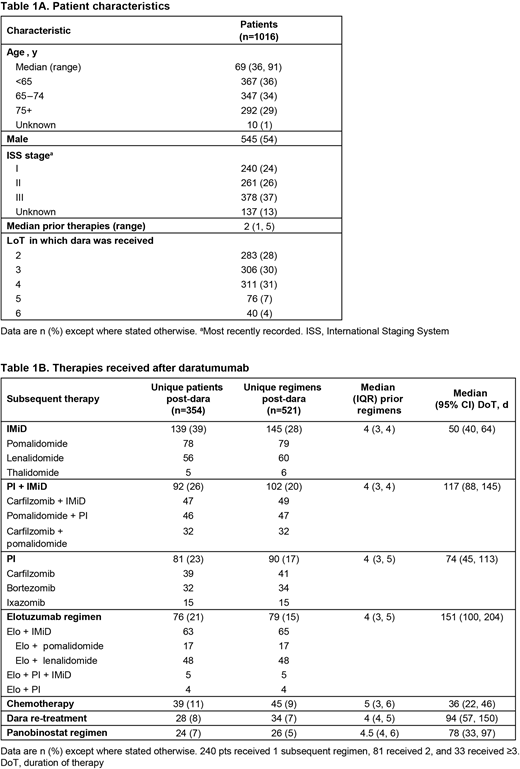
Methods: Pts from the USA aged ≥18 y with RRMM, who received dara in their second to sixth LoT from November 2015 onward, were identified from PREAMBLE (NCT01838512), an ongoing, prospective, observational study, and the McKesson electronic medical record (EMR) database. Pts who had received a prior mAb were excluded. Pts were followed until database lock (PREAMBLE, April 2018; McKesson EMR, May 2018). Baseline demographics and clinical characteristics were assessed using descriptive analysis, and statistical comparisons were made using t or Mann-Whitney U tests (continuous variables) and chi-square tests (categorical variables). Kaplan-Meier analyses were used to estimate duration of therapy (DoT).
Results: In total, 1016 pts received dara as their first mAb in their second to sixth LoT. Baseline characteristics are shown in Table 1A. The most common dara-based regimen was dara plus an immunomodulatory drug (IMiD; 37% of pts, of whom 50% received dara plus pom), followed by dara plus dex and/or chemotherapy (32%), dara plus a PI (27%), dara plus a PI and an IMiD (4%), and dara plus panobinostat (<1%). At database lock, 43% of pts were still on treatment and 35% had switched to subsequent therapy. The most common therapy after dara was IMiDs (as monotherapy or with dex), followed by PI plus IMiD combinations, PIs, and elo-based regimens (Table 1B). Notably, 93% of pts who switched to an IMiD had received an IMiD before dara, and 90% who switched to a PI had received a prior PI. Similarly, most pts who switched to a PI plus IMiD combination had received either an IMiD (88%) or a PI (92%) before dara, and most pts who switched to elo had received an IMiD (91%) or a PI (93%) previously. Pts who switched to an IMiD were also more likely to have received dara plus an IMiD than pts who switched to any other subsequent therapy. There were no clear differences in baseline characteristics among pts who received different classes of therapy after dara; however, pairwise comparisons showed that pts who switched to chemotherapy (p=0.0208) or panobinostat (p=0.0298) had received more prior LoTs than pts who switched to elo-based regimens (Table 1B). Median DoT after dara is shown in Table 1B. Additional data including time to next treatment will be reported at the time of presentation.
Conclusions: In this analysis, pts with RRMM after failure of dara switched to a variety of regimens. The majority received regimens containing IMiDs and PIs despite having been exposed to those agents in the past. Elo-based regimens were received by 21% of pts with RRMM after failure of dara, with most pts receiving elo in combination with len, and were associated with a higher DoT (151 d) after dara than other regimens in this analysis. Elo plus Pd may therefore be an option after dara, as pom is used less frequently in earlier LoTs.
Study support: Bristol-Myers Squibb (BMS). Medical writing: K Tran, Caudex, funded by BMS.
Vij:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Jansson: Honoraria, Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Karyopharma: Honoraria, Membership on an entity's Board of Directors or advisory committees. Chen:Bristol-Myers Squibb: Employment. Yasenchak:Seattle Genetics: Consultancy; Bristol-Myers Squibb: Consultancy. Davis:Bristol-Myers Squibb: Employment.
Author notes
Asterisk with author names denotes non-ASH members.